3 East: Call it the Covid wing
Jennifer Collins will never forget when the third floor of Kootenai Health’s east wing expansion transformed into a COVID-19 isolation unit.
When preparations began, she recalled, “coronavirus” was still a relatively new word in many vocabularies. Precious little information was available and conserving personal protective equipment (PPE) was a high priority.
“We knew it was infectious,” said Collins, who is the 3 East nurse manager at Kootenai Health. “We wanted to make sure we were keeping our staff as safe as possible with the resources available to us.”
The COVID-19 unit has 32 beds. In the event of another surge in coronavirus cases, the unit can accommodate up to 39 patients before needing to expand again.
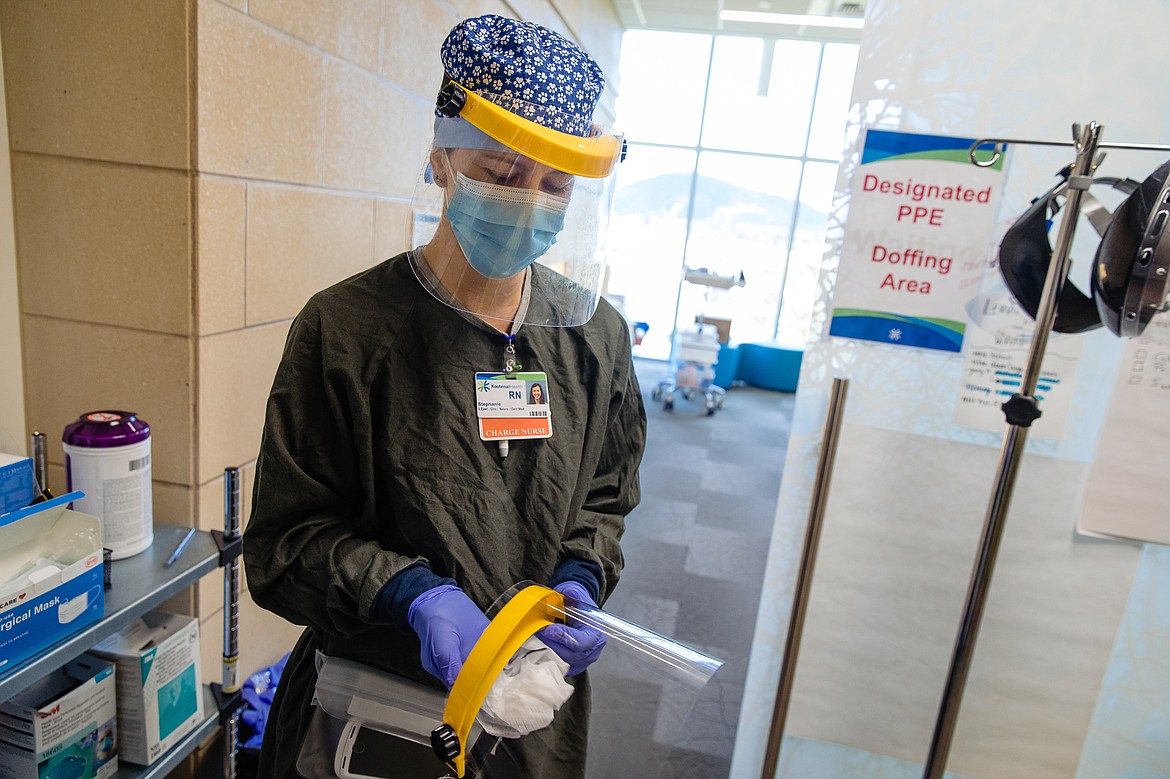
Only essential employees are allowed in the unit. Each person who enters is required to don a gown, gloves, eye protection and a mask.
“It’s hot; it’s uncomfortable,” Collins said. “The gowns go all the way up to your neck. Sometimes it’s a little claustrophobic.”
Staff can’t eat, drink or use the bathroom without removing all their PPE and throwing it away. To minimize waste, staff limit the amount of times they remove their protective equipment.
“They go without those luxuries we take for granted every day, like taking a sip of water,” Collins said.
Even so, PPE requirements aren’t the most painful safety measure necessitated by COVID-19. Director of clinical services Kim Inman said the most “heartbreaking” guideline is the one for visitors.
The virus is so contagious that visitors are not typically permitted to see patients who’ve tested positive.
“That’s way out of our norm,” Inman said. “Families and caregivers provide support and love, which patients need.”
Kootenai Health has invested in technology to help bridge the gap and allow patients to interact with their families. The hospital is also working to make patients feel more at ease and connected to the people caring for them, which can be a challenge when they’re surrounded by fully-garbed medical staff. One option is having physicians wear a photo of themselves so the patients can see what they look like under the mask.
“We wanted to humanize it,” Chief Physician Executive Karen Cabell said.
Under normal circumstances, when a patient is nearing the end of life, family can be there during the final moments. COVID-19 has made that impossible in some cases.
“There are people in our community who have had to say goodbye to their loved ones using technology,” Inman said.
It’s heart wrenching, she said, even for medical staff.
“Maybe our numbers aren’t skyrocketing,” she said. “But for me, as a nurse, it only takes one time to touch my heart.”
The pandemic has taken a heavy toll on health care workers, across the world and here at home. More than 2,100 cases of COVID-19 have been reported among Idaho health care workers, according to the Idaho Department of Health and Welfare.
But the daily risk of infection isn’t the only source of stress. Even after a shift ends, health care workers live with the specter of coronavirus at all times.
“COVID doesn’t go away when we leave work,” said critical care manager Katie Barbera. “There’s not a break when we leave.”
She added that she’d like the community to remember that “an extra dose of kindness helps.”
“You don’t ever really get away from it,” Inman said. “It can be a struggle, because we know what’s happening with our patients here. Then you go out and you see social media and other comments.”
Collins said that teamwork has been essential during the pandemic — not only to manage patient care as new information is discovered about the virus and recommendations frequently change, but also so they can support one another through an unprecedented time.
“Every single one of us has bad days,” Collins said. “We need to be able to lift each other up on bad days, so they can be there to lift us up, too.”
The months since March have been a study in resilience, Barbera said. Health care workers have relied on one another and learned how to manage stress together.
“We’re continuing to pull together as a team as we’re facing it,” she said. “I would struggle much more if I didn’t have such incredible people to work with.”
One of the greatest challenges health care workers have faced is the unpredictable nature of the illness, Cabell said. Patients can decline rapidly within hours.
“The physicians and nurses who are taking care of these patients say it’s different than a patient who comes in with influenza in the winter,” she said.
Though many of the people who have been hospitalized due to COVID-19 are elderly or have preexisting conditions, Cabell noted that younger, otherwise healthy individuals have become seriously ill.
“This is the real deal,” Cabell said. “It’s a serious illness that people need to respect. Although we’ve got some great treatments, it keeps us up at night.”
For all the heartbreak, there have also been moments of joy. Cabell recalled a coronavirus patient who was discharged after a lengthy hospital stay.
“It was very, very exciting as he left,” she said.
Staff played a special song over the intercom as the patient left the unit — a moment of celebration amid so many challenges, one that health care workers hope to repeat.
“We’ve had losses,” Inman said. “Loss of life. Loss of income. It impacts everyone in a different way. But we’ve also had some really great success, too, and we can’t lose sight of that.”